| This is an archive of past discussions. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 20 | Archive 21 | Archive 22 | Archive 23 |
Images in pathophysiology
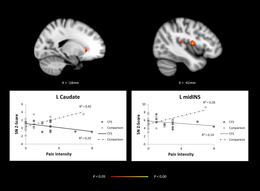
We currently show a brain image that is very difficult to understand. The 2016 primary study uses an unrepresentative definition of CFS, only requiring fatigue (so broader than Fukuda).

I'd like to replace it with an image of a 2-day CPET. Commons has a few images based on primary data. Here, we do have a few more recent reviews explaining these results, for instance the 2024 BMJ practice guidelines. What do you guys think? Maybe the right halve of the image here. The results are a bit different from what MEDRS describe, in the sense that the comparison group is ICF, rather than healthy controls.
The question: Are images (1) subject to the same MEDRS criteria? (2) okay if they give an example of a finding detailed in MEDRS sources? (3) not subject to medrs sourcing requirements? —Femke 🐦 (talk) 17:12, 27 January 2024 (UTC).
- @WhatamIdoing: would you be able to advice? —Femke 🐦 (talk) 20:47, 9 February 2024 (UTC)
- Generally speaking, the purpose of an image is to illustrate existing article content. That illustration can certainly be an example rather than a universal (this apple, not all apples).
- The level of comprehension for the first image here is likely to be approximately "Something about their brains is different", which is not entirely a bad thing. Whichever image you choose (or if you decide to use both), I'd suggest keeping the captions simple and direct. Perhaps as simple as "Research has found differences in the brain network activity", without mentioning the age of the study participants, control groups, or anything "technical". The second image could have a caption that says something like "When they exercise two days in a row, ME/CFS people get worse on the second day." (Or whatever the point of the illustration is.) WhatamIdoing (talk) 23:27, 9 February 2024 (UTC)
Rewrite of history section
While I always prefer to write sections collaboratively, I decided to rewrite this in one go, as there was significant WP:COPYVIO, which I didn't want to keep on the page for longer than necessary. I think it's okay 4 out of 5 paragraphs are mostly based on the IOM report, since that is an excellent and neutral history of ME and CFS. Very happy to get feedback on that or any other part of the rewrite.
I'm aware of overlap with the controversy section. I may rewrite that too at some point, but I think you can't write a history of ME/CFS without the psychological controversy. —Femke 🐦 (talk) 19:59, 5 February 2024 (UTC)
- Added some detail changes. May be too technical for some readers, I don't know. Ward20 (talk) 21:01, 5 February 2024 (UTC)
- The IOM report does not include these details, at least around the antibody titer. Can you ensure the text matches the source? Or find another secondary source on the history? —Femke 🐦 (talk) 21:08, 5 February 2024 (UTC)
- Added source[1] pg 155-158. I can probably find another if the John Hopkins University press book is not sufficient. Ward20 (talk) 02:18, 6 February 2024 (UTC)
- The IOM report does not include these details, at least around the antibody titer. Can you ensure the text matches the source? Or find another secondary source on the history? —Femke 🐦 (talk) 21:08, 5 February 2024 (UTC)
- I'm very happy with your revisions. The new history section covers everything important. The Quirky Kitty (talk) 03:07, 10 February 2024 (UTC)
Steps before GA nomination
I think the article is close to meeting the GA criteria now. I hope to bring the article up to FA level, and want to make sure the article is at least comprehensive before nominating for GA, so that we can get feedback on the entire article. Two questions for talk page watchers:
- What should I do to prepare
- Do people want to be co-nominators? In particular, @Ward20 and @The Quirky Kitty?
On my to-do list before I nominate is a rewrite of three bits:
- The causes section, and non-viral triggers like stress, pregnancy and mold.
 Done
Done - The neuro-inflammation paragraph (which relies too much on an older work for NPOV)
- The research section, which has overlap with the pathophysiology section and for which the James Lund Alliance paper is better than the MPDI journal. The NIH research roadmap (to be published in May), will allow for an ever better section likely.
- Finish the signs and symptoms section with description of debilitating fatigue, pain and sleep problems.
 Done
Done
What else should we tackle before a nomination? —Femke 🐦 (talk) 13:58, 10 February 2024 (UTC)
- I would be honored be nominate this article with you. The Quirky Kitty (talk) 14:06, 10 February 2024 (UTC)
- Thank you for the opportunity to participate and I will do what I can, although my time to edit is a bit spotty at the moment. I just did a reread and besides what has been listed I would suggest:
- Revisit the time for diagnosis. It is somewhat incomplete in the article and the literature is murkey because CDC says six months, NICE says three months and to treat as soon as possible for children. Other sources say prompt appropriate treatment can reduce the scope of the illness and even improve prognosis. I think it's an important aspect to present properly in the article.
- The article uses treatment and management interchangeably and it could be somewhat confusing to the reader. I have some difficulty conceptionally with it in the article, but sometimes I'm over-analytical.
- I think the controversy section needs some rework. The pace trial was arguably as controversial as XMRV. The controversy sub article is quite well done, but there's been such an amount of controversy it may take consensus about how much to cover. I like how the sub article presents the items under tiles such as Recognition, Contrasting viewpoints, XMRV retrovirus, PACE trial, Support for patients and Historical perceptions. I suggest bringing research funding under controversy. I suggest adding the conflict of interest of the disability benefit government programs and insurance companies over the definitions and classification of the illness that reduced financial disbursements.
- Ward20 (talk) 10:24, 11 February 2024 (UTC)
- That's really useful. I will definitely include more about delays in diagnosis. I've recently added it to the prognosis section, and will also add it to the diagnosis section from that angle.
- I think we are shooting ourselves in the foot with our section on proposed treatments. The suggested headings in WP:MEDORDER are either management or treatment, where management is preferred over treatment for chronic conditions. I do not believe it is quite neutral to put graded exercise therapy in the table of contents, as people might easily skip over the work proposed, and believe GET is a treatment option recommended in clinical guidelines.
- Conversely, people only reading the cognitive behaviour therapy may come away with a very negative idea about CBT in general, rather than the more nuanced view found in the management section (useful for coping and insomnia).
- Your suggestion to put the pace trial in the controversy section may resolve our disagreement from before: that way we can give due attention to graded exercise therapy, without suggesting the therapy is still included in clinical guidelines. —Femke 🐦 (talk) 13:28, 11 February 2024 (UTC)
- About the PACE trial, more mainstream sources discuss the methodological flaws in the trial [2], the Freedom of information requests, and how scientists were reprimanded by the tribunal for exaggerating harassment f.i. [3]. I've seen a conflict-of-interest angle from patient organisations and more niche scientific journals, but I find the sources insufficient from a BLP point of view. When we make strong accusations about living people, the sources need to be due without a doubt.
- The BLP policy also covers talk pages by the way. This means that you should always use of high-quality source when discussing these issues even on talk. Of course you didn't name names here, but they are not too hard to guess. —Femke 🐦 (talk) 17:15, 11 February 2024 (UTC)
- No, I wasn't thinking about individual conflict of interest, More about CoI of Government and insurance agency's historical denial of disability claims based on a lack of a conclusive test. Also, denial and time limits on payments (usually 24 months) by claiming the illness is a mental disorder. This material has some coverage in the controversy sub article.
- Thank you for the opportunity to participate and I will do what I can, although my time to edit is a bit spotty at the moment. I just did a reread and besides what has been listed I would suggest:
- I just did a quick Google search and a large amount lawyer websites appeared. To my surprise, some actually stated that some disability insurance policies now have exemptions to coverage or time limitations on coverage (24 months) if you're diagnosed with chronic fatigue syndrome, similar to diagnosis for a mental disorder. "The evolution of denying fibromyalgia and chronic fatigue syndrome claims in group long term disability policies". I don't expect that is a good reliable source, but I will dig into the matter further to look for scholarly articles. Ward20 (talk) 22:31, 11 February 2024 (UTC)
- Ah, that makes sense, sorry for the misunderstanding. I don't think there is a lot of controversy over this in media. A better location may be in the social and economic impact subsection instead. This is going to be really tough to write from a global perspective, as the US has a "unique" health care system, so results from the US cannot be assumed to be generalisible. —Femke 🐦 (talk) 17:55, 12 February 2024 (UTC)
- I misread your point about time for diagnosis. I've added a sentence about delays in diagnosis, but that wasn't what you meant.
- The way to incorporate this is to change from bullet points with intricate details of the diagnostic criteria, to an assessment on how they are different. For instance, which are research vs clinical diagnostic criteria, and how does that impact their formulation (clinical criteria will have an earlier presumtive diagnosis, given that you don't want to withhold care while investigating). The 2024 BMJ source gives some nice pointers here. Maybe I'll cultivate some patience and rewrite this too before a GA nom. —Femke 🐦 (talk) 19:58, 21 February 2024 (UTC)
- Ah, that makes sense, sorry for the misunderstanding. I don't think there is a lot of controversy over this in media. A better location may be in the social and economic impact subsection instead. This is going to be really tough to write from a global perspective, as the US has a "unique" health care system, so results from the US cannot be assumed to be generalisible. —Femke 🐦 (talk) 17:55, 12 February 2024 (UTC)
- I just did a quick Google search and a large amount lawyer websites appeared. To my surprise, some actually stated that some disability insurance policies now have exemptions to coverage or time limitations on coverage (24 months) if you're diagnosed with chronic fatigue syndrome, similar to diagnosis for a mental disorder. "The evolution of denying fibromyalgia and chronic fatigue syndrome claims in group long term disability policies". I don't expect that is a good reliable source, but I will dig into the matter further to look for scholarly articles. Ward20 (talk) 22:31, 11 February 2024 (UTC)
Controversy section
My proposed rewrite of the controversy section. I've decreased the overlap with the history section, and have increased overlap with the "proposed treatments" section, in the hope we can move towards removing that section. I have also removed the mentiono of the newsweek article, which is old news, and included a summary of the PACE controversy.
We didn't have an article on outcome switching yet, which I remedied yesterday. I'm quite shocked to see how common it is, and how often study authors defend the practice when called out on it.
ME/CFS is a contested illness, with debates mainly revolving around the cause of the illness and treatments.[1] Historically, there was a heated discussion whether the condition was psychological or neurological.Lim and Son Professionals who subscribed to the psychological model had frequent conflicts with patients, who believed their illness to be organic.[2] While ME/CFS is now generally believed to be a multisystem neuroimmune condition,Lim and Son a subset of professionals still see the condition as psychosomatic, or an "illness-without-disease".[2]
In 2009, the journal Science[3] published a study that identified the XMRV retrovirus in a population of people with CFS. Other studies failed to reproduce this finding,[4][5][6] and in 2011, the editor of Science formally retracted its XMRV paper[7] while the Proceedings of the National Academy of Sciences similarly retracted a 2010 paper which had appeared to support the finding of a connection between XMRV and CFS.[8]
Treatments based on behavioural and psychological models of the illness have been the subject of much contention. The largest clinical trial on behavioural interventions, the 2011 PACE trial, concluded that graded exercise therapy and CBT are moderately effective. The trial drew heavy criticism.[1] The study authors changed the definition of recovery during the trial, which led some patients to be classified as recovered at the start of the trial. A reanalysis under the original protocol showed no significant difference in recovery rate between treatment groups and controls.[9]
Open questions:
- I don't like how the second paragraph flows. Maybe we can summarise this further, since it's 15 years ago? But how to connect that sentence to other text?
- I don't the 2013 Speight article is sufficiently reliable, will add something about patients being disbelieved to social impact section. Does that work? I found a recent scoping review on internet use that talks about this; mainly about people not being believed by their community. The doctor-patient section already talks about how doctors disbelieve patients.
References
- ^ a b Blease C, Geraghty KJ (September 2018). "Are ME/CFS Patient Organizations "Militant"? : Patient Protest in a Medical Controversy". Journal of Bioethical Inquiry. 15 (3): 393–401. doi:10.1007/s11673-018-9866-5. PMID 29971693.
- ^ a b O'Leary D (December 2020). "A concerning display of medical indifference: reply to 'Chronic fatigue syndrome and an illness-focused approach to care: controversy, morality and paradox'". Medical Humanities. 46 (4): e4. doi:10.1136/medhum-2019-011743. PMID 32601171.
- ^ Lombardi VC, Ruscetti FW, Das Gupta J, Pfost MA, Hagen KS, Peterson DL, et al. (October 2009). "Detection of an infectious retrovirus, XMRV, in blood cells of patients with chronic fatigue syndrome". Science. 326 (5952): 585–589. Bibcode:2009Sci...326..585L. doi:10.1126/science.1179052. PMC 3073172. PMID 19815723. (Retracted, see doi:10.1126/science.334.6063.1636-a)
- ^ Erlwein O, Kaye S, McClure MO, Weber J, Wills G, Collier D, et al. (January 2010). Nixon DF (ed.). "Failure to detect the novel retrovirus XMRV in chronic fatigue syndrome". PLOS ONE. 5 (1): e8519. Bibcode:2010PLoSO...5.8519E. doi:10.1371/journal.pone.0008519. PMC 2795199. PMID 20066031.
- ^ Groom HC, Boucherit VC, Makinson K, Randal E, Baptista S, Hagan S, et al. (February 2010). "Absence of xenotropic murine leukaemia virus-related virus in UK patients with chronic fatigue syndrome". Retrovirology. 7 (1): 10. doi:10.1186/1742-4690-7-10. PMC 2839973. PMID 20156349.
- ^ van Kuppeveld FJ, de Jong AS, Lanke KH, Verhaegh GW, Melchers WJ, Swanink CM, et al. (February 2010). "Prevalence of xenotropic murine leukaemia virus-related virus in patients with chronic fatigue syndrome in the Netherlands: retrospective analysis of samples from an established cohort". BMJ. 340: c1018. doi:10.1136/bmj.c1018. PMC 2829122. PMID 20185493.
- ^ Alberts B (December 2011). "Retraction". Science. 334 (6063): 1636. Bibcode:2011Sci...334.1636A. doi:10.1126/science.334.6063.1636-a. PMID 22194552.
- ^ Lo SC, Pripuzova N, Li B, Komaroff AL, Hung GC, Wang R, Alter HJ (January 2012). "Retraction for Lo et al., Detection of MLV-related virus gene sequences in blood of patients with chronic fatigue syndrome and healthy blood donors". Proceedings of the National Academy of Sciences of the United States of America. 109 (1): 346. Bibcode:2012PNAS..109..346.. doi:10.1073/pnas.1119641109. PMC 3252929. PMID 22203980.
- ^ Vink M, Vink-Niese A (May 2022). "The Updated NICE Guidance Exposed the Serious Flaws in CBT and Graded Exercise Therapy Trials for ME/CFS". Healthcare (Basel, Switzerland). 10 (5). doi:10.3390/healthcare10050898. PMC 9141828. PMID 35628033.
((cite journal)): CS1 maint: unflagged free DOI (link)
—Femke 🐦 (talk) 19:40, 18 February 2024 (UTC)
- I concur with the changes above and with reworking the XMRV part. I do have a couple of suggestions.
- The sentence,
"The study authors changed the definition of recovery during the trial, which led some patients to be classified as recovered at the start of the trial"
might be clearer with wording similar to,"The study authors changed the definition of recovery during the trial, which increased the number of recovered patients at the conclusion of study. Due to the changed recovery definition, some patients met the recovery criteria at the start of the intervention."
- A condensed XMRV section could be included in the paragraph along with material about viruses similar to:
"Human herpesviruses, Ross River virus, Enteroviruses, and Human parvovirus B19 have long been associated with ME/CFS in studies, but none of these viruses could be associated with a majority of patients. These viruses may cause illness in patient subgroups, or they might be hit-and-run triggers for ME/CFS.[4] One viral study caused considerable controversy by establishing a causal relationship between ME/CFS and the retrovirus XMRV.[5] Some with the illness began taking AIDS drugs[6], and national blood supplies were suspected to be tainted with the retrovirus. After several years of study, the XMRV findings were determined to be the result of contamination of the testing materials.[7]"
Ward20 (talk) 07:07, 21 February 2024 (UTC)- I've asked chatgpt to reword more concisely (I erred in the opposite direction), and we came up with
The study authors changed the criteria for recovery, leading to more recovered patients by the end of the trial. Some patients even met the criteria at the intervention's outset.
- As for the XMRV study, the Panelli study is primary and published in a Frontiers journal, so not great. Which is a shame, as your text is excellent. The Rasa study is a great addition to the 'viral and other infections' subsection, where I've added it to replace a source with WP:Integrity issues. I think we'd need a shorter introduction into that section, something like: "The possible role of chronic viral infection in ME/CFS has been a subject of debate" (cite Rasa).. The only thing we still need a high-quality reliable source for the XMRV stuff. —Femke 🐦 (talk) 19:32, 21 February 2024 (UTC)
- Added secondary sources for the XMRV material. I think that the last sentence about PACE should be a bit more specific,
After the change, some patients even met the criteria at the intervention's outset.
Ward20 (talk) 04:26, 22 February 2024 (UTC)
- Added secondary sources for the XMRV material. I think that the last sentence about PACE should be a bit more specific,
- I've asked chatgpt to reword more concisely (I erred in the opposite direction), and we came up with
Treatment section, revisited
Now that our management section is in a reasonable condition, and we discuss former treatments in the controversy section, I'd like to reopen the discussion of bringing the article more in line with WP:MEDORDER. Medorder suggests that management is typically the best option when talking about chronic illnesses. The key reasons I would like to follow MEDORDER here are:
- I think having proposed treatments is not neutral. People may come away with the idea these are actual treatments, or close to being approved. CBT as treatment and GET are controversial and better discussed in context of non-controversial talking therapy and exercise / in the controversy section. In Wikiwand, the AI sometimes summarises the article as supporting GET and CBT as treatment, which a sloppy / brainfogged reader will likely do to.
- Ampligen is considered "emerging" per the BMJ source, not mentioned in 2021 Mayo, not mentioned in the main NICE guidelines, mentioned as one of many drugs in their pharmaceutical evidence review, and also one among many in the German HTA. I would like to move it to the research section, making that a full sentence, rather than a short sentence. Putting it in its own subsection is undue weight.
—Femke 🐦 (talk) 18:54, 23 February 2024 (UTC)
- If that makes the present status of those issues clearer to understand I concur. Ward20 (talk) 04:40, 25 February 2024 (UTC)
MEDRS question: CDC publishing in MDPI
This study came out today: "Heterogeneity in Measures of Illness among Patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Is Not Explained by Clinical Practice: A Study in Seven U.S. Specialty Clinics" [8]. It's in a special issue focusing on ME/CFS in MDPI's Journal of Clinical Medicine. I know that some MDPI journals are viewed as deserving of a better reputation than it's carried, or at least some titles. I haven't had a chance to look at this, and as it may be considered a primary source, it may well not merit consideration for the article, at least at this point. But while I have seen a number of ME/CFS publications in this and other MDPI journals over the past couple of years, I was wondering if that was raising the credibility of the journal(s), or reducing the potential impact of the papers themselves considerably.
But, seeing the CDC--well, it's part of the Multi-Center ME/CFS outfit that's been going for some time, and the first several authors are CDC--choose to publish this here is something I'm curious about. Lead author is Elizabeth Unger, head of the ME/CFS division at CDC for over a decade. Does any of this matter? I've seen so much very specific MEDRS-related criticism when it comes to journals with questionable histories, as well as rebukes of criticisms of the CDC over the years. If it strikes anyone as meaningful...should it be brought to the attention of those on WP who render judgments on these matters? NeurastheniaMilkshake (talk) 07:04, 29 February 2024 (UTC)
- Cool study. Like you said, it's a primary source, and therefore we should not cite it. Generally, about the reliability of MPDI and Frontiers journals: guidelines already says we should evaluate them case-by-case. For instance, we have cited MPDI journals when they reported the results from the EUROMENE consortium, as these are published in the better MPDI journals, are from a highly-regarded consortium, and importantly, are frequently cited by sources we consider highly reliable. Scopus provides a ranking of journals, with the Journal of Clinical medicine ranking 137/830 in the category of general medicine. If it's top 50%, it's usually fine, even though the more controversial a statement, the stronger our sourcing needs to be. Special issues typically bring their own issues: normal editors are replaced by invited editors, who may not have the same standards in accepting papers. I believe current guidelines strike a good balance between caution, and flexibility. —Femke 🐦 (talk) 08:20, 29 February 2024 (UTC)
- Thanks for calling attention to the study. After reading it, my impression is the same as Dr. Bateman's. "Bateman says the study was well executed and comprehensive, but she doesn't see anything groundbreaking. However, she's hopeful the data will serve as a "foundation" for future research."[9] Ward20 (talk) 23:45, 1 March 2024 (UTC)
Removing lead citations?
At FAC, editors often prefer to omit citations from the lead. This makes the text easier to read, and citation aren't quite necessary per WP:LEADCITE. With a more controversial article like this, this is very much a trade-off, as the lead may be more subject to IP editing if there are not citations in the lead. What do you guys think? —Femke 🐦 (talk) 11:49, 3 March 2024 (UTC)
- My preference would be to remove the double cited instances when possible, and also the cites for non-controversial material. I would leave cites on controversial material based on previous experience of editors tagging sentences based upon what they may have read about outdated medical opinions. Ward20 (talk) 19:11, 3 March 2024 (UTC)
Nice Recommendations [10]
The article presently cites this source about 20 times in about five different ways. I'm not sure what the best way of approaching this is for the good article nomination. Ward20 (talk) 00:38, 4 March 2024 (UTC)
- For the good article nomination, this is okay. For the FAC, we'll need consistent citations. I think citing the pdf version is easiest, as we can use the page numbers then. —Femke 🐦 (talk) 08:08, 4 March 2024 (UTC)
The duration ... is unpredictable
@Ward20: the duration being unpredictable does not seem to be supported by the source. It even contradicts the next sentence that says recovery is rare. If recovery is rare, it follows that predictability about illness duration is high: you'll have a ~95% chance of being correct when you say it's lifelong.
I'm removing all the unnecessary MPDI and Frontiers journal articles. Some are useful to meet the comprehensiveness criterion, such as the EUROMENE one and the review on reproductive health and ME/CFS. We may get pushback at FAC when we rely on these journals too much, as sources are supposed to be high-quality reliable sources there. The 2021 Mayo Clinic source contains information about prognosis that supports the statement on recovery being rare. —Femke 🐦 (talk) 17:29, 4 March 2024 (UTC)
Discussion of psychosocial risk factors in "viral infections" section
Currently we have the following text:
A systematic review found that fatigue severity was the main predictor of prognosis in CFS, and did not identify psychological factors linked to prognosis. Another review found that risk factors for developing post-viral fatigue or CFS after mononucleosis, dengue fever, or Q-fever included longer bed-rest during the illness, poorer pre-illness physical fitness, attributing symptoms to physical illness, belief that a long recovery time is needed, as well as pre-infection distress and fatigue. The same review found biological factors such as CD4 and CD8 activation and liver inflammation are predictors of sub-acute fatigue but not CFS.
This one paragraph is really out of line with the overall tone of the article (that ME/CFS is a serious medical condition) and goes way against the broader consensus. If we discuss this at all, we should say it's controversial. The Quirky Kitty (talk) 05:55, 6 March 2024 (UTC)
- This is a difficult one. The source is slightly older than ideal (2017). However, I don't see many sources that directly contradict this paper. If you look at a paper that came out two days ago (Table 1, the LC-only entries), you see multiple predictive biological factors have been found for long COVID, making it likely that these will be found in ME/CFS. But no direct comparison or contradiction..
- This contrasts with how we've dealt with the issue in different locations of the article:
- In the paragraph on onset in the cause section, we've given multiple sources for % of infectious onset. It's a bit messy, but doesn't put undue attention on the IoM numbers which included very low % too, which I guess are from BPS studies
- In the GET paragraph, we first have a statement on the clinical guidance (GET no longer advised), and then we delve deeper saying studies disagree on whether there is a small effect or no effect.
- —Femke 🐦 (talk) 18:37, 6 March 2024 (UTC)
GA Review
The following discussion is closed. Please do not modify it. Subsequent comments should be made on the appropriate discussion page. No further edits should be made to this discussion.
| GA toolbox |
|---|
| Reviewing |
- This review is transcluded from Talk:Myalgic encephalomyelitis/chronic fatigue syndrome/GA1. The edit link for this section can be used to add comments to the review.
Reviewer: Maxim Masiutin (talk · contribs) 15:30, 8 March 2024 (UTC)
Hello, Femke, Ward20 and The Quirky Kitty! Thank you for you work on the article and for nominating it.
I review the revision 1212410967 https://en.wikipedia.org/w/index.php?title=Myalgic_encephalomyelitis/chronic_fatigue_syndrome&oldid=1212410967
On references, the reference for PMID 28033311 is duplicated: one with name "r", another with name "pmid28033311", but even the quote is the same in both ("The highest prevalence of illness is in persons aged 40–50 years...")
On date format, please consider consistent date format use in citations, i.e. the dates formatted according to the "DMY" (Day Month Year) style that you selected. While most of the dates are in the DMY format, such as "22 February 2024", there are a few instances of the YYYY-MM-DD format (an ISO 8601 format): "2024-04-02", "2011-06-01", "2024-02-22".
The use of references in the lead is not consistent: either all claims in the reference should be backed up by references, or no references at all should be used in the lead, in this case the lead should repeat all the claims made in the body where they are referenced. The first paragraph in the lead does not have any reference (while the other paragraphs have references). This paragraph does not have references: "Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating long-term medical condition. People with ME/CFS experience flare-ups of the illness or crashes following minor physical or mental activity. This is known as post-exertional malaise (PEM) and is the hallmark symptom of the illness."
On lead size in paragraphs: the lead should have at most 4 paragraphs, while technically the lead has 5 paragraphs.
- While I'm all up for a four-paragraph lead, the actual guidance is more flexible: WP:LEADLENGTH. If the lead remains manageable, an occasional 5-paragraph lead is okay if that works better with organisation. For instance, if you have 5 distinct topics to work with. —Femke 🐦 (talk) 11:19, 9 March 2024 (UTC)
- Don't worry, I got it down to 4 paragraphs. The Quirky Kitty (talk) 13:20, 9 March 2024 (UTC)
On grammar, in the first paragraph of the lead there is the following text: "Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating long-term medical condition. People with ME/CFS experience flare-ups of the illness or crashes following minor physical or mental activity. This is known as post-exertional malaise (PEM) and is the hallmark symptom of the illness.", but it may be unclear what "This" in the last sentence refers to; please consider rewriting the sentence/paragraph to remove the unclear reference. The pronoun "This" in the last sentence could refer to either "flare-ups of the illness or crashes" or "minor physical or mental activity", which can cause confusion. Here's a possible rewrite to clarify the reference: "Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating long-term medical condition. People with ME/CFS experience flare-ups of the illness or crashes. These symptoms, known as post-exertional malaise (PEM), typically follow minor physical or mental activity and are the hallmark symptom of the illness." In this revised version, "These symptoms" clearly refer to "flare-ups of the illness or crashes," and it's specified that they follow minor physical or mental activity. This should eliminate any ambiguity.
Also, there are spelling errors:
- "unavaible" (sic),
- use of curly apostrophe instead of the straight one in violation of the Manual of style ("people’s")
- "targetting" -- is it a British spelling? Does the article uses British or American English? Please consider using either British or American English and declare which one did you use via a template, such as ((Use American English|date=March 2024))
On wikilinks, please also try to avoid piped wikilinks in the lead, as they may be misleading in Wikipedia. For example the word "mechanisms" is linked, but the reader, when clicking it, goes to a Wikipedia article about "pathophysiology". Piped wikilinks should be avoided because …they can create confusion for the reader. The reader might expect to be directed to a page that directly corresponds to the linked text, but instead, they are taken to a different page with a different title. This discrepancy can disrupt the reader’s understanding and flow of reading. Instead, consider using direct links to the relevant Wikipedia articles. If the term "pathophysiology" is more accurate, use that term directly in the text and link it to its corresponding Wikipedia page. This way, the reader knows exactly what to expect when they click on a link: our goal is to make information as accessible and understandable as possible for all readers. I also found wikilinks on terms mold and pregnancy, which are probably the commonly understood terms and should not be wikilinked. There are no specific dictionary on which terms are considered commonly understood by a broad audience, but generally, terms that are part of everyday language or basic education are considered common knowledge. For instance, words like "water", "book", and so on, are universally understood and do not require wikilinks. However, the decision to wikilink a term can also depend on the context and the intended audience of the text. If the text is intended for a specialized audience, such as a scientific research paper, it might be appropriate to wikilink terms that are common in that field but not necessarily understood by the general public. In the case of "mold" and "pregnancy", while these terms are generally understood, they may or may no encompass broad topics with many subtopics that readers might or might not want to explore further. Therefore, wikilinking them could or could not provide valuable additional information to the reader: I am not sure about that, I just raised my concerns of these words, ultimately, the decision to wikilink a term should be guided by whether it enhances the reader’s understanding of the text, as it is always a good idea to consider the potential benefits to the reader and balance them against the risk of overloading the text with unnecessary links.
On the terms in the lead that are hard to understand: the word "pathophysiology" may not be understood by a general audience, it might be beneficial to provide a brief, simplified explanation of the term within the article (you can refer to review PMID: 37838675 when adding details on pacing). You can make explanations for specific terms, making them easier to understand, in parentheses immediately after the term is first used, or a synonym can be used instead that can be easier to understand, even a few simpler words that aim to have the same meaning. Also, there is a term "orthostatic intolerance" is used in the lead without immediate explanation or clarification on what is it: this is a medical term that might be difficult for some readers to understand. Also, there are terms: "Pacing and activity management", which, in the context of ME/CFS, refer to specific strategies for managing the condition, however, they might not be clear to all readers, as they are not immediately explained.
On clinicians' awareness, it is mentioned in the article that clinicians may be unfamiliar with ME/CFS, as it is often not covered in medical school, still, there is no official disease in the international classification of diseases such as ICD-10 or ICD-11, therefore, the question arises on why do the clinicians have to know about the disease if it is does not officially exists in the ICD? It is not explicitly mentioned in the article that ME/CFS as a disease exists (described) in peer-reviewed literature, and there are clinical practice guidelines or similar documents, for example, the CDC provides information for healthcare providers on ME/CFS, including assessment, managing symptoms, and providing other supportive strategies to improve patients’ quality of life: https://www.cdc.gov/me-cfs/healthcare-providers/index.html ; besides that, the National Health and Medical Research Council (NHMRC) in Australia recommended updating the Australian clinical guidelines and selected three international guidelines for interim use, as described by ME/CFS South Australia Inc, a Registered Charity: https://mecfssa.org.au/resources/clinical-guidelines-including-diagnostic-criteria ; also the National Institute for Health and Care Excellence (NICE) in the UK has guidelines for diagnosing and managing ME/CFS in children, young people, and adults: https://www.nice.org.uk/guidance/ng206 ; also the US ME/CFS Clinician Coalition provides resources for medical providers caring for people with ME/CFS: https://www.cdc.gov/me-cfs/healthcare-providers/clinical-care-patients-mecfs/index.html ; therefore, in the case of conditions like ME/CFS that are not included in the ICD, information can often be found in scientific literature, clinical case reports, and guidelines or consensus documents published by professional organizations, so that clinicians can also learn from their colleagues' experiences and from patients themselves; the absence of a condition from the ICD does not mean it doesn't exist or is not valid, as provided by the documents mentions; the ICD is updated periodically, and conditions can be added as more is learned about them and as their recognition in the medical community grows -- this can be the explanation why the clinicians should be aware of ME/CFS, i.e. this information may serve grounds for the imperative for the clinicians to be aware of this condition, as I said earlier, while the lack of formal education and recognition in the ICD can make it more challenging for clinicians to learn about conditions like ME/CFS, there are still many resources available for those who seek to understand and help their patients with these conditions and that it underscores the importance of continuous learning in the medical profession. Please consider adding these clinical practice guidelines in the article as grounds for the clinicians to know about this disease.
- A statement such as "ME/CFS is real" is not neutral imo, as it uses the frame of a disease which may not exist. Compare with a statement such as "climate change is real", which you see in click-baity news articles. In the scientific literature on climate denial, this is considered poor science communication, as this pre-supposed there is a (valid) disagreement on the existence of climate change. The literature on ME/CFS clearly says ME/CFS is included in the ICD, even though it's included under the two subparts of the name. We already mention the NICE guidelines and the CDC in the next. The fact we refer to these guidelines already implies they exist, it is unnecessary to include more explicit sentences. —Femke 🐦 (talk) 11:02, 9 March 2024 (UTC)
On broad coverage of the topic: please consider explaining the link between Post-Infectious Neurological Syndromes (PINS) and ME/CFS. Post-Treatment Lyme Disease (PTLD), among others. Is ME/CFS a type of PINS or they are separate independent diseases? If ME/CFS is a type of PINS with Epstein-Barr virus often as a trigger? This virus, and the long covid were mentioned in the Viral infections subsection, but not the notion of Post-Infectious Neurological Syndromes (PINS). Please consider explaining this notion.
- I hadn't heard of PINS before today; none of the sources I'm aware of describe ME/CFS as a PINS, even though post-infectious ME/CFS might be one. I didn't find any sources when I searched PINS and ME/CFS together on PubMed, or when searching ME/CFS and "Post-Infectious Neurological Syndromes", using the standard filters (<5 years, reviews). Therefore, I do not believe it WP:DUE. We embarrasingly don't have an article on PTLDS, only on chronic Lyme (which is basically the same, except people who use the term believe in ineffective treatments..). I've added a paragraph to the classification section explaining the link with post-acute infection syndromes, which also encompasses PTLDS and long COVID. Hope that addresses your point. —Femke 🐦 (talk) 11:58, 9 March 2024 (UTC)
Please also consider mentioning whether study long COVID may contribute to understanding of ME/CFS, and vice versa, in the section on the research direction, if that is covered by significant sources, such as reputable reviews.
The article is verifiable, it contains no original research, no copyright violation and no plagiarism, it is broad in coverage, by addressing the main aspects of the topic, it stays focused on the topic, it is neutral, stable and properly illustrated.
However, I have concerns on whether the lead section is easily understandable by a broad audience, and whether it complies on the Manual of Style in some instances I mentioned earlier. Looking forward for your reply.
Maxim Masiutin (talk) 19:46, 8 March 2024 (UTC)
- Thanks for the review. Really appreciate the comments that exceed the GA criteria, as we're slowly prepping for FA. I'm a bit ill at the moment, but hope to make a proper start tomorrow.
- ME/CFS is included in the ICD, and has been since 1969. What in the text makes you believe it isn't? The fact that ICD-10 didn't have the code for CFS, only for ME? —Femke 🐦 (talk) 20:12, 8 March 2024 (UTC)
- My comments fit the GA criteria in part, and exceed in part: for example, comments on grammar or manual of style fit the GA criteria, while other comments such as on completeness do not prevent the article from complying to the GA criteria, however, the GA criteria mention that the article should be broad in its coverage (it addresses the main aspects of the topic), and there is wide margin on appreciation, one reviewer may consider some information sufficient while another reviewer may consider the same information insufficient, however, there should be common sense, and we should keep in mind that the GA review is a lightweight process, still, important topics should be covered. If you state that ME/CFS is included in the ICD, and has been since 1969, please specify that in the article and give reliable sources, as the article currently states the following (quote): "In the ICD-10, only (benign) ME was listed, and there was no mention of CFS." Besides that, the article lists the following: "ME/CFS has been classified as a neurological disease by the World Health Organization (WHO) since 1969, initially under the name benign myalgic encephalomyelitis. Even though the cause of the illness is unknown, symptoms indicate a central role of the nervous system. Alternatively, based on abnormalities of immune cells, it has been classified as a neuroimmune condition. In the WHO's most recent classification, the ICD-11, both chronic fatigue syndrome and myalgic encephalomyelitis are listed under the term post-viral fatigue syndrome. They are classified as other disorders of the nervous system." Therefore, the article does not mention that the exact name "Myalgic encephalomyelitis/chronic fatigue syndrome" is classified in the ICD. The scientific articles and clinical practice guidelines list explicit sequence of 5 words "Myalgic encephalomyelitis/chronic fatigue syndrome", but not the ICD. Maxim Masiutin (talk) 20:25, 8 March 2024 (UTC)
- Hello, Femke, Ward20 and The Quirky Kitty, the GA maintenance bot is not fully running today, see may be running at erratic times today Maxim Masiutin (talk) 20:13, 8 March 2024 (UTC)
- Thanks for looking at the article. I'm going through some of the simpler fixes right now. As for citations in the lead, let's include them. This is a medical article and many aspects of the disease have been disputed. The Quirky Kitty (talk) 03:51, 9 March 2024 (UTC)
- @The Quirky Kitty if you wish to keep them, please add a citation for the first paragraph that lacks citations. Maxim Masiutin (talk) 07:05, 9 March 2024 (UTC)
- I did that, and couldn't find any other uncited statements. The Quirky Kitty (talk) 07:33, 9 March 2024 (UTC)
- Thank you! I did minor edits to my initial review: they don't alternate the meaning, and are mostly technical. Maxim Masiutin (talk) 07:37, 9 March 2024 (UTC)
- I saw that in the words that differ between British and American spelling, there were more British-spelled words, so I put the template to use British English and replaced the American-spelled words to their British counterparts. According to WP:GAN/I#R3, "In the case of a marginally non-compliant nomination, if the problems are easy to resolve, you may be bold and fix them yourself." Maxim Masiutin (talk) 08:00, 9 March 2024 (UTC)
- I see that you resolved all the significant issues except the use of the following complex terms in the lead:
- pacing and activity management
- orthostatic intolerance
- MOS:INTRO states the following:
Make the lead section accessible to as broad an audience as possible. Where possible, avoid difficult-to-understand terminology, [...] Where uncommon terms are essential, they should be placed in context, linked, and briefly defined. The subject should be placed in a context familiar to a normal reader.
Maxim Masiutin (talk) 08:09, 9 March 2024 (UTC)- I fixed that shortly after you sent this message. Femke addressed several more of your concerns, and I'm seeing what else I can fix up. The Quirky Kitty (talk) 13:18, 9 March 2024 (UTC)
- I did that, and couldn't find any other uncited statements. The Quirky Kitty (talk) 07:33, 9 March 2024 (UTC)
- @The Quirky Kitty if you wish to keep them, please add a citation for the first paragraph that lacks citations. Maxim Masiutin (talk) 07:05, 9 March 2024 (UTC)
Changes for easier reading and better understanding by a broad audience
I made a few changed for easier reading and better understanding by a broad audience, without altering the meaning. Some changes are related to replacing piped wikilinks links to simple "as is" wikilinks, as it usually makes reading easier and understanding easier. If you don't like particular changes, feel free to restore how the content was, however, please keep in mind that we write for general audience, not for health care professionals. Thank you! Maxim Masiutin (talk) 01:00, 10 March 2024 (UTC)
- Ward20, as you see, removing piped wikilinks and replacing them to simple wikilinks without pipe is not a panacia, but it is a good practice and in many cases it can make understanding of things easier. In this particular case, it was a sentence "The 1994 CDC criteria, sometimes called the Fukuda criteria...." and when I click to this wikilink to find more about this criteria, I got to the page on Keiji Fukuda and there were no single word about this criteria. So I changed the sentence to "The 1994 CDC criteria, sometimes called the Fukuda criteria (named after Keiji Fukuda, an epidemiologist)" and things became much more clearer and straigforwad, don't you think so? Please let me know what you thing? I made the similar on retroviral drugs and retroviruses. Your opinion on my changes are very appreciated. I read The Economist newspaper from time to time, the "Science and technology section", and they are very good on explaining complex things in simple language, so I made those changes in a similar way. They had a recent article related to ME/CFS when they described complex things very clearly, see https://www.economist.com/science-and-technology/2024/02/21/long-covid-is-not-the-only-chronic-condition-triggered-by-infection Maxim Masiutin (talk) 01:32, 10 March 2024 (UTC)
- Yes, I did see that the changes made the material easier to understand, flow much better and the links make more sense. I didn't notice anything in the changes that weren't improvements. Thanks. Ward20 (talk) 02:11, 10 March 2024 (UTC)
Co-nomination
I know that two people were GA co-nominators; I don't know how this will be handled/counted, I just used regular GA review workflow. Maxim Masiutin (talk) 01:02, 10 March 2024 (UTC)
- Nothing extra to do here. Co-nominations are not counted officially. —Femke 🐦 (talk) 07:08, 10 March 2024 (UTC)
DYK suggestions
We're allowed one sentence on the front page at WP:DYK, @The Quirky Kitty & @Ward20. What would you guys like to highlight? A few options, but I'm not good in finding interesting things:
Did you know that..
- ... the emergence of long COVID has sparked increased interest in myalgic encephalomyelitis/chronic fatigue syndrome?
- ... many people with long COVID develop myalgic encephalomyelitis/chronic fatigue syndrome?
- ... some people with severe myalgic encephalomyelitis/chronic fatigue syndrome can lose the ability to speak?
- ... that per healthy life year lost, research funding for myalgic encephalomyelitis/chronic fatigue syndrome is only 3-7% of what the average condition gets?
—Femke 🐦 (talk) 18:12, 9 March 2024 (UTC)
- The second bullet point by far. Ward20 (talk) 20:40, 9 March 2024 (UTC)
- Either 2 or 4. However 4 feels a bit preachy. Like we're advocating for increased funding. I don't think that's the purpose of DYK. The Quirky Kitty (talk) 08:17, 10 March 2024 (UTC)
- I've done 2, 4, 3, in that order :). Thanks for the input! —Femke 🐦 (talk) 08:50, 10 March 2024 (UTC)
PINS
The post-infections neurological syndrome (PINS) which is a relative condition to ME/CFS is mentioned in the following reviews:
You may also find some information in the following research studies:
- doi:10.1212/WNL.0b013e3182840b95
- doi:10.1177/1756286420952
- doi:10.1186/s13052-021-00968-y
- doi:10.1007/s13365-020-00941-1
- doi:10.1212/01.wnl.0000179302.93960.a
- doi:10.1016/j.jinf.2009.02.011
All these studies may contribute to the completeness of the article on ME/CFS, because ME/CFS is supposed to be a neurological disorder caused by neuroinflammation after an infection.
Also, there are some drugs that supposedly reduce neuroinflammation, such as modafinil. Many scholars belive that modafinil indeed reduced neuroinflammation, however, they mostly refer to an invitro lab experiments, still a study PMID 16272188 suggests that chronic modafinil may not be beneficial in patients with chronic fatigue syndrome, but there are other causes by chronic fatigue syndrome, not just ME.
So, thank you for working on this article, this is a very important topic and research on this topic will bring significant benefits. Maxim Masiutin (talk) 01:44, 10 March 2024 (UTC)
- The recent review does not mention myalgic encephalomyelitis (it's about acute disseminated encephalomyelitis & variants). The 1997 review I can't access, but is from 1997. I do not believe this to be due still. —Femke 🐦 (talk) 08:24, 10 March 2024 (UTC)
- Indeed, there is no clear explicit link between PINS and ME/CFS in the medical literature, I tried to find but didn't find a solid link. The only more or less solid link was in the Economist which is a weekly newspaper, not a peer-reviewed jounal:
Many researchers suspect, for example, that what is variously labelled chronic-fatigue syndrome or myalgic encephalomyelitis (ME) is such a post-infectious neurological syndrome (PINS). However, a suggestion that Epstein-Barr virus is the trigger has never been nailed down. Much remains mysterious about the condition itself, and, with at least nine different proposed definitions, it may well be that the umbrella term encompasses different conditions with overlapping symptoms and varied causes.
https://www.economist.com/science-and-technology/2024/02/21/long-covid-is-not-the-only-chronic-condition-triggered-by-infection -- this is an article from February 21, 2024. - There are a few peer-reviewed article where both terms (PINS and ME/CFS) exist, but they exist in different paragraphs and are not explicitly linked correctly, and we should not speculate. There are more articles exists where PINS is mentioned, but without ME/CFS, so we should not make our own conclusions. Therefore, let us avoid describing PINS until we get a solid article with explicit link Maxim Masiutin (talk) 11:04, 10 March 2024 (UTC)
- Indeed, there is no clear explicit link between PINS and ME/CFS in the medical literature, I tried to find but didn't find a solid link. The only more or less solid link was in the Economist which is a weekly newspaper, not a peer-reviewed jounal:
Better explanation of symptoms
There is a sentence that is not easy to understand, I suggest you find a way to improve it, I mean the following sentence:
"Symptoms triggered by sitting or standing up, memory and concentration problems, and pain are common."
This sentence is not specific enough. It is unclear what symptoms are being triggered by sitting or standing up. A more precise sentence would specify the symptoms that occur upon standing or sitting up, such as dizziness or fainting. For example, "Symptoms like dizziness triggered by sitting or standing up, memory and concentration problems, and pain are common". This provides a clearer picture of the condition being described.
I have another idea: "Symptoms such as dizziness that worsens with moving from lying down or sitting to standing, problems with memory or thinking skills, and pain are common".
What do you think?
I decided to discuss this topic outside the scope of the GA review, because there is always limitless ways to improve an article. Maxim Masiutin (talk) 16:30, 9 March 2024 (UTC)
- Or even a better version that has better flow: " "Symptoms such as dizziness that worsens with moving from lying down or sitting to standing, problems with memory or thinking skills, and pain are common in ME/CFS." Maxim Masiutin (talk) 16:31, 9 March 2024 (UTC)
- Better like this? The orthostatic intolerance can happen when people sit up, not only stand up. —Femke 🐦 (talk) 16:37, 9 March 2024 (UTC)
- You can describe it better, I just spotted a sentence that was not very good because the ""Symptoms triggered by ..." was unclear in regards to what symptoms were meant. Maxim Masiutin (talk) 19:19, 9 March 2024 (UTC)
- I went to the page and found the sentence "Further common symptoms include dizziness or nausea when sitting or standing up, along with memory and concentration issues, and pain." which is much better than it was before, thank you! Maxim Masiutin (talk) 19:21, 9 March 2024 (UTC)
- Nitpick here. I believe "standing" is a better word than "standing up" in this case. "Standing up" often means rising to one's feet rather than standing still. As I recall, the objection to "standing" was that it could also mean "walking", but I have rarely seen "standing" used in that way. "Standing" seems to be better defined as a stationary position.[11] The citation[12] uses "standing", not "standing up", and in another source,[13] "In up to 95% of those with ME/CFS, an immobile, upright position (eg, prolonged standing or sitting will cause or worsen symptoms.)" Ward20 (talk) 20:37, 9 March 2024 (UTC)
- Ah, I hadn't thought of it like that. I take your point that standing up is not ideal here. I was maybe thinking too much of POTS, which is a change in heart rate when you go from lying/sitting to standing. —Femke 🐦 (talk) 08:43, 10 March 2024 (UTC)
- Nitpick here. I believe "standing" is a better word than "standing up" in this case. "Standing up" often means rising to one's feet rather than standing still. As I recall, the objection to "standing" was that it could also mean "walking", but I have rarely seen "standing" used in that way. "Standing" seems to be better defined as a stationary position.[11] The citation[12] uses "standing", not "standing up", and in another source,[13] "In up to 95% of those with ME/CFS, an immobile, upright position (eg, prolonged standing or sitting will cause or worsen symptoms.)" Ward20 (talk) 20:37, 9 March 2024 (UTC)
- Better like this? The orthostatic intolerance can happen when people sit up, not only stand up. —Femke 🐦 (talk) 16:37, 9 March 2024 (UTC)
- I think it looks good. I was the one who changed "orthostatic intolerance" to "symptoms when sitting or standing" but I don't mind adding an explanation as well. My goal was to respond to your GA feedback quickly, not reach absolute perfection. The Quirky Kitty (talk) 11:52, 10 March 2024 (UTC)